Australia’s antibiotic misuse spreads superbug fears; Doctors worry over hospitals’ inappropriate prescriptions
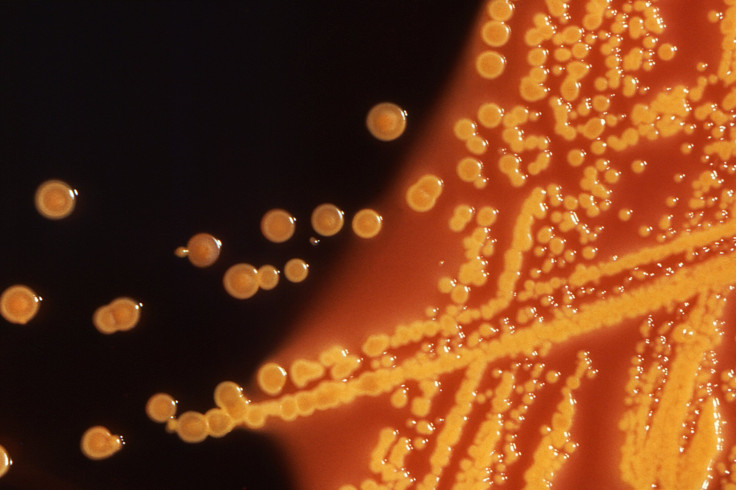
Australian nursing homes may be contributing to the creation of antibiotic-resistant superbugs. Results of a survey have revealed some grave figures as hospitals continue to inappropriately prescribe antibiotics to patients. The drug is being wrongly prescribed in up to 20 percent of cases, the survey revealed.
It has been found out that many residents were on prolonged prescriptions of antibiotics for unclear reasons. This is very concerning as frequent and inappropriate use of antibiotics can lead to antimicrobial-resistance that creates superbugs.
Professor Karin Thursky from the National Centre for Antimicrobial Resistance Stewardship said that Australian nursing homes mostly prescribed antibiotics for soft-tissue, skin, respiratory and urinary infections. However, one in five patients was given the drug as preventative measures.
Nearly 22 percent of prescriptions were handed over to residents without any symptom or sign of infection in the week before they started the course of antimicrobial medication. About two-thirds of the prescriptions were considered inappropriate even when patients did show certain symptoms of infection.
“The big issue for us is that we know that if you're continually exposed to antibiotics and you select out what we would call a multi-resistant organism, it's not just that patient that's at risk, it's actually the other patients in the facility that are at risk,” Thursky told the ABC.
He added that there were multiple reasons for incorrect prescriptions of the drugs. Lack of documentation justifying their use, lack of review and omission of start and end date were some of the reasons pointed out. In some cases the drugs were taken for “indications that didn't meet any of the standard indications.”
The pilot survey included 180 nursing homes across all Australian states and was carried out from June to August 2015. On the day of the survey, 11.3 percent of the residents were on antibiotic, although only 4.5 percent showed signs and symptoms of infection.
Project Officer Dr. Noleen Bennett from the National Centre for Antimicrobial Resistance Stewardship said that even though senior staff in aged care facilities was better aware of antimicrobial resistance, in certain groups of workers, knowledge of superbugs remained comparatively low.
The World Health Organisation (WHO) has declared antibiotic-resistance as one of the greatest threats to human health.





















