By adding new genetic code, Swiss scientists coax stem cells from body fat to turn into insulin-making beta cells
Fat is largely to blame for the large number of Type 2 diabetes cases, but Swiss scientists just discovered that stem cells taken from love handles could bring researchers close to creating a personal repair kit for diabetics.
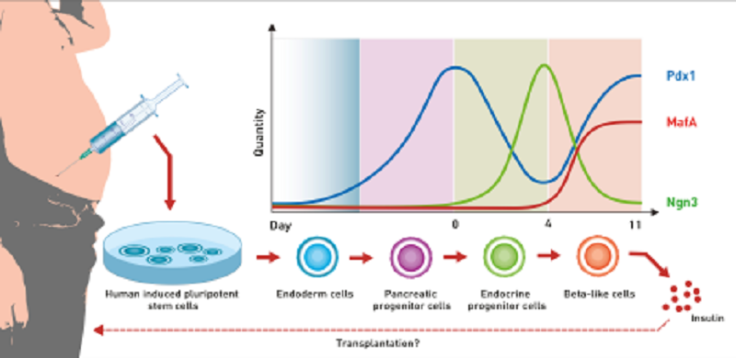
Researchers at the Swiss Federal Institute of Technology (ETH) in Zurich harvested stem cells from a 50-year-old man’s body fat and coaxed the cell to turn it into beta cells that produce insulin by the addition of a new genetic code. The code triggers the same process that happens in the pancreas where the beta cells are produced, reports The Telegraph.
The scientists, based in Basel, added the genetic software, a highly complex synthetic network of genes, which they designed to recreate the key growth factors involved in the maturation process. These growth factors are Ngn3, Pdx1 and MafA, the concentration of which change during the differentiation process.
These natural processes must be reproduced as close as possible to produce functioning beta cells. “The timing and the quantities of these growth factors are extremely important,” says Martin Fussenegger, professor of biotechnology and bioengineering at ETH Zurich’s Department of Biosystems Science and Engineering and lead researcher.
The beta cells are then transplanted back into the diabetic where it is expected to clear out sugar as normal. Although the team used liposuction to remove the fat – which contains a lot of stem cells – from the patient, not much is needed. Fussenegger points out that “Most people have an overabundance of fat from which these stem cells can be harvested."

Fussenegger adds that using the new technique, researches could implant new functional beta cells in diabetics made from their own adipose tissue. This would do away with the need to suppress the immune system of the recipient because it would use endogenous cell materials taken from the patient’s own body.
ETH Zurich, which published the study on Nature Communications journal, plan to start human trials within as short as five years. Success could mean no more daily insulin injections for millions of diabetics around the world.





















