The Science Behind Near Death Experiences Explained In A Study
When a person is nearing death, the general focus of the health care team goes to the heart, and in ways that can sustain its function. Because the conventional medical theory in these events is the heart supplies other organs, and when it stops beating, the entire body will falter too.
The Proceedings of the National Academy of Sciences published a study that involved a scientific monitoring of the heart and brain activity of rats before it dies from hypoxia. In the study, it was found that the brain sent a surge of signals to the heart, causing it to weaken further. But when these signals were barred, the heart activity improved. The journal then suggests that if the same process is true for humans, then severing the pathway through which these signals travel can prolong the human heart.
Jimo Borjigin, a neuroscientist at the University of Michigan Medical School in Ann Arbor, who co-authored the study, said, "People naturally focus on the heart, thinking that if you save the heart, you'll save the brain. You have to sever [the chemical communication between] the brain and heart in order to save the heart." He adds that this new discovery refutes the majority of present medical practices.
According to the American Heart Association, the annual incidence of cardiac arrest in America is approximately 400,000, and only 10 percent of these patients are able to survive and be discharged from the hospital after medical treatment. The team then aimed to discover how a completely healthy heart suddenly goes into arrest only after a few minutes of oxygen decline.
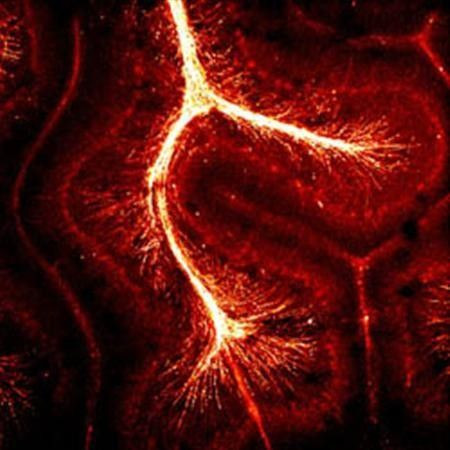
The study was conducted by inducing cardiac arrest in rats through lethal injection and carbon dioxide inhalation. The team then analysed the the brain and heart activity through electroencephalography (EEG) and echocardiography (ECG) , respectively. The researchers also noted the chemical substances that sent and received signals in the both the brain and the heart.
During the initial phase of the experiment, the heart rates of the rats declined significantly, but the brain continuously projected a strong connection with the heart. This part of the study was conducted through a new technology that intricately measured the heart rate of the rats, beat by beat.
This finding suggests that although an individual loses consciousness during a cardiac arrest, the brain does not stop functioning. In fact, it keeps on working and sending off signals to save the heart, as published in a study by Borjigin’ team in the PNAS in 2013. Borjigin said that these mechanisms may answer the phenomenon behind “realer than real near-death experiences.”
The flood of dopamine and other neurochemicals during cardiac arrest causes the individual to have feelings of pleasure and alertness. In rats, this brain and heart connection continued until the heart started going on a ventricular fibrillation, which is the declination the lower heart chamber’s contractility, and subsequent cessation of the heart to pump blood.
However, further into the study, the researchers barred the chemical flow between the brain and the heart by cutting the rats’ spinal cords. The act delayed ventricular fibrillation, and the animals’ lives were prolonged three times more than those whose spinal cords were not severed.
Borjigin, howeve, said that this experiment was done in rats, and the implication of this study is yet to be determined in humans. But if scientists can find a way to block the chemical pathway between the brain and the heart through drugs, and not through spinal cord cutting, then it may be possible to prolong the lives of patients undergoing cardiac arrest.
To contact the writer, email rinadoctor00@mail.com




















