Researchers develop painless smart cell patch of insulin-producing beta cells to control diabetes
University of North Carolina (UNC) and North Carolina State University researchers have developed a synthetic patch that has natural beta cell which secretes doses of insulin. The patch, a painless method of delivering insulin, aims to control blood sugar levels of diabetic on demand, minus the risk of inducing hypoglycemia.
Scientists have actually been attempting for years to duplicate the function of beta cells that produce the insulin. However, in diabetics, the beta cells do not work properly. Until the patch was developed, the usual method of delivering insulin was through injections that are painful.
Medical News Today notes that another alternative was to transplant normal beta calls, but the procedure runs the risk of rejection or side effects from immunosuppressive therapies.
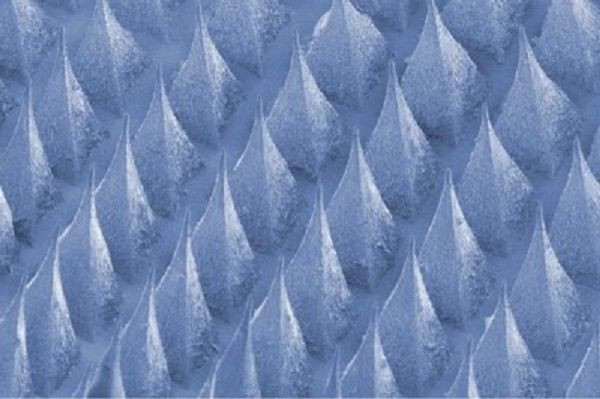
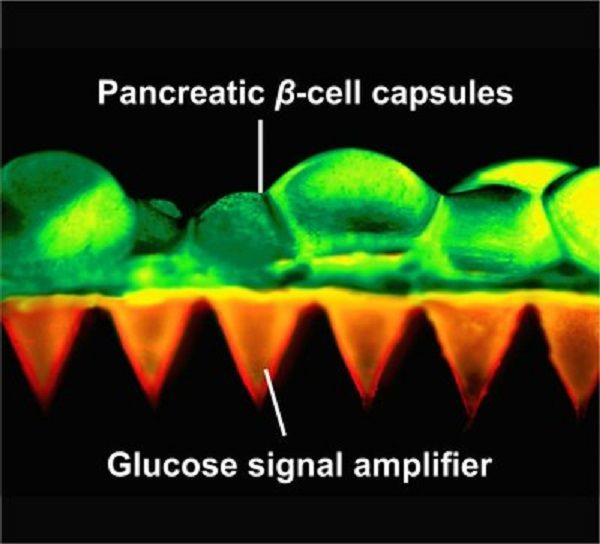
The patches, reported in 2015 in the Proceedings of the National Academy of Sciences, they developed are thin polymeric squares filled with tiny needles, similar to a miniature bed of nails. The size of a quarter coin, the new smart patch integrates the needles – about the size of eyelashes - with live beta cells unlike previous models in which the needles had manmade bubbles of insulin.
The patch was tested on small animals with Type 1 diabetes and it showed quick response of very high blood sugar levels which remained significantly lower, at a time, up to 10 hours. Dr Zhen Gu, assistant professor of the joint department of biomedical engineering of the two universities, says, “This study provides a potential solution for the tough problems of rejection, which has long plagued studies on pancreatic cell transplants for diabetes.”
Zhen adds, “Plus it demonstrates that we can build a bridge between the physiological signals within the body and these therapeutic cells outside the body to keep glucose levels under control.”
Yanqi Ye, lead author, constructed the smart cell patches that uses natural material found in cosmetic and diagnostics. She also created glucose-signal amplifiers, synthetic nanovesicles with three chemicals that ensures the cells could “hear” the call from increasing blood sugar levels and respond accordingly.
While hundreds of diabetics have undergone transplant of human beta cells since the procedure was introduced in 1990, only few of the patients who undergone the procedure achieved normal blood sugar levels. Most of the transplants were rejected or a lot of the drugs taken to suppress the immune system interfere with the beta cells and insulin activities.
Dr John Buse, co-author of the study, published in Advanced Materials, and professor of medicine at the UNC School of Medicine, says the smart patches give some diabetics time off over their diabetes self-care – often on 24/7 basis. “It would not be a cure but a desperately needed vacation,” he says.





















